If you’ve ever experienced persistent redness, bumps, and irritation on your face, you may be familiar with the frustration and embarrassment that comes with living with rosacea.

This chronic skin condition affects millions of people around the world, and while it can be a source of discomfort and self-consciousness, it is important to understand that it is not contagious and can be managed with proper treatment and self-care. In this article, we’ll delve into the symptoms, causes, and treatment options for rosacea, so you can take control of your rosacea and feel confident in your own skin.
Symptoms of Rosacea
Rosacea is characterized by redness, flushing, and bumps on the face, particularly on the nose, cheeks, and forehead. Symptoms of rosacea may include:
- Redness and flushing of the skin
- Bumps and pimples on the face
- Visible blood vessels on the face
- Dry, rough skin
- Swelling or thickening of the skin, particularly on the nose
- Burning or stinging sensations on the face
- Eye irritation, including redness, dryness, and swollen eyelids
What Causes Rosacea?
The exact cause of rosacea is not fully understood, but a number of factors are thought to contribute to the development of the condition. These include:
- Genetics: Some people may be more prone to developing rosacea due to their family history.
- Environmental factors: Exposure to wind, cold, or hot temperatures, as well as certain skin care products and makeup, may trigger flare-ups of rosacea.
- Microorganisms: The presence of certain bacteria and mites on the skin may contribute to the development of rosacea.
- Vascular abnormalities: Rosacea may be caused by abnormal blood vessels in the face, which can cause flushing and redness.
- Immune system: Some research suggests that an overactive immune system may contribute to the development of rosacea.
Treating Rosacea
There is no cure for rosacea, but there are several treatment options that can help manage the condition and reduce the frequency and severity of flare-ups. These may include:
- Topical medications: Creams and gels that contain ingredients such as metronidazole and azelaic acid can help reduce redness and inflammation.
- Oral medications: Antibiotics such as doxycycline and tetracycline may be prescribed to help reduce inflammation and clear up bumps on the skin.
- Laser treatment: Laser therapy can help reduce the appearance of redness and visible blood vessels on the face.
- Self-care: In addition to medical treatment, there are several self-care measures that can help manage rosacea. These may include avoiding triggers that can cause flare-ups, using gentle skin care products, and protecting the skin from the sun.
Who Gets Rosacea?
While rosacea can affect people of all skin tones and hair colors, it is more commonly seen in people with lighter skin, particularly those who have fair or very fair skin. It is also more common in people who have red or blond hair, as well as those who have blue or green eyes.
However, it is important to note that rosacea can affect anyone, regardless of their skin tone or hair color. It is a chronic skin condition that is thought to be caused by a combination of genetic and environmental factors. If you are concerned about the possibility of having or developing rosacea, it is important to speak with a dermatologist who can help you understand your risk factors and provide guidance on how to manage the condition.
Subtypes of Rosacea
There are several subtypes of rosacea that can affect different areas of the body. The most common subtypes of rosacea include:
Erythematotelangiectatic Rosacea
Erythematotelangiectatic rosacea is a subtype of rosacea that is characterized by redness, flushing, and visible blood vessels on the face. It is often accompanied by a burning or stinging sensation on the skin, as well as dryness and roughness.

This subtype of rosacea is the most common and tends to affect people in their 30s and 40s. It is more commonly seen in women and people with fair skin, but it can affect anyone, regardless of their skin tone or gender.
Treatment options for erythematotelangiectatic rosacea may include topical medications, oral medications, laser treatment, and self-care measures such as avoiding triggers that can cause flare-ups and using gentle skin care products. It is important to work with a dermatologist to determine the most appropriate treatment plan for your individual needs.
If you have erythematotelangiectatic rosacea and are experiencing redness, flushing, and visible blood vessels on the face, it is important to speak with a dermatologist for proper diagnosis and treatment. With proper management, it is possible to control the symptoms and improve the appearance of the skin.
Papulopustular Rosacea
Papulopustular rosacea is a subtype of rosacea that is characterized by redness, swelling, and bumps (papules and pustules) on the skin, particularly on the nose, cheeks, and forehead. It is often accompanied by a burning or stinging sensation on the skin, as well as dryness and roughness.

This subtype of rosacea also tends to affect people in their 30s and 40s and again, is more commonly seen in women. And like erythematotelangiectatic rosacea, it is also more commonly seen in people with fair skin, but it can affect anyone, regardless of their skin tone or gender.
In addition to redness, swelling, and bumps on the skin, papulopustular rosacea may also cause acne-like breakouts. The bumps may be filled with pus, which is why this subtype is sometimes referred to as “acne rosacea.” Unlike acne, however, papulopustular rosacea is not caused by clogged pores and is not responsive to over-the-counter acne treatments.
Papulopustular rosacea tends to come and go in cycles, with flare-ups occurring every few weeks or months. It is important to work with a dermatologist to develop a treatment plan that can help reduce the frequency and severity of flare-ups. This may include the use of medications to reduce inflammation and clear up bumps on the skin, as well as self-care measures.
If you have papulopustular rosacea, it is important to speak with a dermatologist for proper diagnosis and treatment. With proper management, you can control the symptoms and improve the appearance of your skin.
Phymatous Rosacea
Phymatous rosacea is a subtype of rosacea that is characterized by thickening and swelling of the skin, particularly on the nose. This thickening of the skin can cause the nose to become enlarged and distorted, a condition known as rhinophyma. Phymatous rosacea can also cause bumps and irregular surface nodules on the skin.
This subtype of rosacea is more commonly seen in men, and it tends to develop over time. It is often accompanied by other symptoms of rosacea such as redness, flushing, and bumps on the skin.
Treatment options for phymatous rosacea may include laser treatment to reduce the thickness of the skin and improve the appearance of the nose, as well as oral and topical medications to reduce inflammation. In some cases, surgery may be recommended to remove excess tissue and restore the normal shape of the nose.

Image Source: DermatologyAdvisor.com
If you have phymatous rosacea and are concerned about the appearance of your skin, it is important to speak with a dermatologist for proper diagnosis and treatment. With proper management, it is possible to control the symptoms and improve the appearance of the skin.
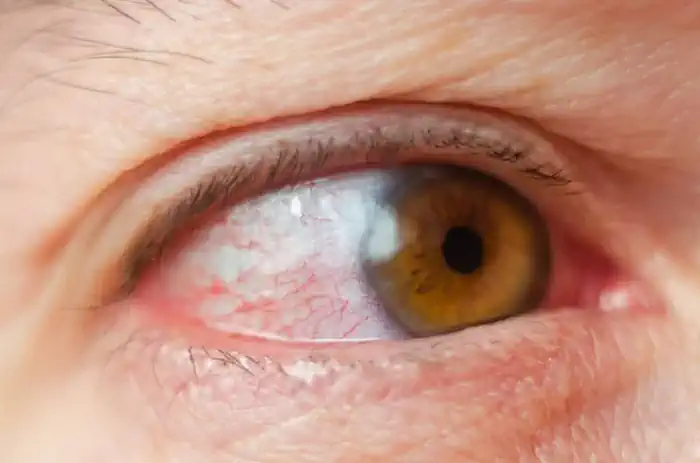
Ocular Rosacea
This subtype is characterized by eye irritation and other symptoms that affect the eyes.
In addition to causing redness, bumps, and irritation on the skin, rosacea can also affect the eyes. This is known as ocular rosacea, and it can cause a range of symptoms including:
- Redness and swelling of the eyelids
- Dryness and burning sensations in the eyes
- Sensitivity to light
- Blurred vision
- The feeling of a foreign object in the eye
- Tearing
Ocular rosacea can be uncomfortable and may lead to additional problems such as sties and eye infections if left untreated. It is important to seek medical attention if you are experiencing any of these symptoms, as proper treatment can help prevent further complications.
If you have rosacea and are experiencing eye irritation or other symptoms of ocular rosacea, it is important to speak with a dermatologist or an eye specialist (ophthalmologist) for proper diagnosis and treatment. Treatment options for ocular rosacea may include the use of artificial tears, warm compresses, and oral or topical medications to reduce inflammation and manage symptoms. In some cases, laser treatment may also be recommended.
It is important to note that individuals with rosacea may experience symptoms of more than one subtype. For example, someone with erythematotelangiectatic rosacea may also experience symptoms of ocular rosacea. It is important to speak with a dermatologist to determine the appropriate treatment plan for your specific subtype of rosacea.
There are several factors that can trigger flare-ups of rosacea, including:
- Alcohol consumption
- Hot drinks or spicy foods
- Exposure to extreme temperatures (such as hot or cold weather)
- Sun exposure
- Stress
- Certain medications (such as steroids or blood pressure medications)
- Skincare products or makeup that contain alcohol or fragrances
- Exercise
- Hot baths or showers
- Emotional upset
It is important to note that triggers can vary from person to person, and what may cause a flare-up in one individual may not have the same effect on another. It is helpful to keep a journal to track what triggers your flare-ups and to avoid those triggers as much as possible. It is also important to speak with a dermatologist about your specific triggers and to develop a plan to manage your rosacea.
See a Dermatologist
If you think you may have rosacea, it is important to see a dermatologist for proper diagnosis and treatment. While rosacea cannot be cured, with proper management, you can control the symptoms and lead a happy, healthy life.

